Omega-3 & COVID-19: What the Studies Say
How does nutrition impact COVID-19? That’s a question many people have pondered since the pandemic reared its ugly head in 2020.
Two years later, the topic is just as relevant. Experts agree that COVID-19 will likely be with us for years to come. And be it COVID-19 or other diseases, the world needs more ways to thwart harmful microbes. Diet and supplements may never replace vaccines, drugs, and other treatments. But if they could give us a better fighting chance, they might be a helpful (and affordable) adjunct.
At Omega3 Innovations, we’ve been keeping tabs on the COVID-19 research for omega-3 fatty acids, vitamin D and melatonin in particular. These nutrients clearly influence our immune health, although exactly how they perform in clinical settings is still being studied.
In a four-part series, we’re going to tackle how these nutrients work alone and together to fight infections. First up to bat, let’s focus on omega-3s – a key player in our cells.
NOTE: Vitamins and supplements do not take the place of getting vaccinated or following other precautions, like wearing masks and social distancing.
Why Scientists Think Omega-3s May Help
There are many reasons scientists have hypothesized that omega-3s could help against COVID-19.
For one, past studies of other diseases have found that omega-3s benefited patients struggling with complications from Acute Respiratory Distress Syndrome [1, 2, 3]. If omega-3s helped in those cases, scientists hypothesize the benefits might apply to COVID-19, too.
Scientists have also called out how these fatty acids work at the cellular level. Notably, omega-3s:
• Protect the cells’ lipid metabolism, which has implications for viral spread.
• Reduce inflammation, which could lessen the risk of complications.
• Promote healthy cell signaling, which may reduce viral entry and support the body’s immune response.
All these mechanisms have the potential to influence the severity of COVID-19 – and so, let’s take a closer look at how they work.
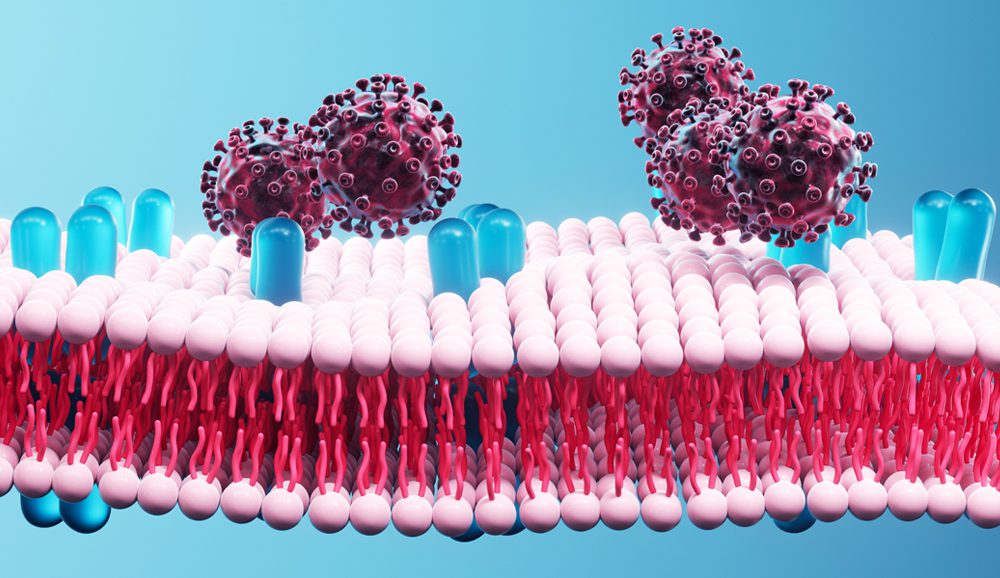
The entry point: To get into our cells and spread, viruses have to penetrate the cell membrane. The fats in our cell membranes influence how susceptible we are to viral attacks and how well our immune system responds.
Omega-3s May Block Viruses from Usurping Our Fats
When you get an infection, viruses rely on fats (i.e. lipid molecules) to spread. Viruses depend on fats to cross into the host cell membrane. And, once a virus gets into the cell, they can reprogram the fat metabolism to favor virus replication [2, 4].
The devious ways viruses manipulate our fats is common to many types of infections – and COVID-19 is no exception. Indeed, several studies have shown that COVID-19 can change a patient’s lipid profile. What’s more, how much the virus messes with a patient’s lipids correlates with disease severity [4].
Omega-3 fatty acids – specifically the two called EPA and DHA – are important for maintaining a healthy fat balance in the cell membranes. EPA and DHA also inhibit SREBP transcription, which is one of the key ways that viruses reprogram the cells’ fat metabolism [2, 4]. For that reason, scientists speculate omega-3s may weaken the virus’ ability to replicate and spread.
Omega-3s Fight Inflammation
The symptoms of COVID-19 can range from none to life-threatening. But big problems arise when the body’s inflammatory response goes haywire.
Uncontrolled inflammation can lead to organ damage and other serious complications. That’s why many COVID-19 treatments focus on reducing inflammation.
Omega-3s have well-known anti-inflammatory effects, through several different means:
Reduce Pro-Inflammatory Cytokines & Oxylipins
High doses of omega-3s can reduce the production of pro-inflammatory cytokines, like interleukin-6 [5]. This is important, since pro-inflammatory cytokines play the lead role in the deadly cytokine storm.
Omega-3s reduce other types of inflammatory substances, too! For instance, when a person consumes more EPA and DHA, arachidonic acid levels decrease. Lower levels of arachidonic acid in turn lowers the levels of pro-inflammatory oxylipins [1].
High levels of oxylipins are linked with severe COVID-19 infections (as well as many heart health issues) [6, 7]. For that reason, having lower levels of these inflammatory baddies is thought to be best for survival and recovery.

A hallmark of inflammation: Having too high levels of the pro-inflammatory interleukin-6 can be harmful. Fortunately, omega-3s have been found to help lower interleukin-6 levels.
Boost Production of Anti-Inflammatory SPMs
EPA and DHA also serve as the building blocks to important molecules called resolvins, protectins, and maresins. These molecules do exactly what their names imply: They resolve and protect against excessive inflammation.
In animal studies, these inflammation-fighting omega-3 derivatives have been shown to improve infection outcomes [8].
While human trials are still underway, one small-scale study from England hinted at their importance: It found that patients who died from COVID-19 produced markedly fewer resolvins and protectins compared to those who survived [9].
Omega-3s Promote Healthy Cell Signaling
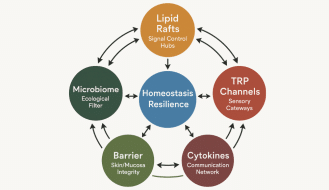
When you eat omega-3s, these fatty acids collect in the cell membranes of all your tissues. This strategic position matters. The cell membrane is the entry point for viruses and bacteria into the cell. Plus, it’s where the cell’s surface receptors – the cells’ communication tools – hang out.
The surface receptors are, in large part, contained within the lipid rafts inside the cell membrane. Increased age, obesity, diabetes, and heart disease reduce the quality of the fats inside the lipid rafts, which in turn, reduces the receptors’ ability to function. Omega-3s, on the other hand, help clean up the fats inside these lipid rafts.
By mucking out the wrong kinds of fats (like cholesterol) from the lipid rafts, omega-3s may have indirect effects, such as:
Reducing viral entry into the cell
Studies of several coronaviruses show that having less cholesterol in the lipid rafts decreases viral entry [11]. And one recent in vitro study found that EPA inhibited the COVID-19 virus’ ability to attach to the ACE2 receptor [10]. More studies replicating these results are needed, however.
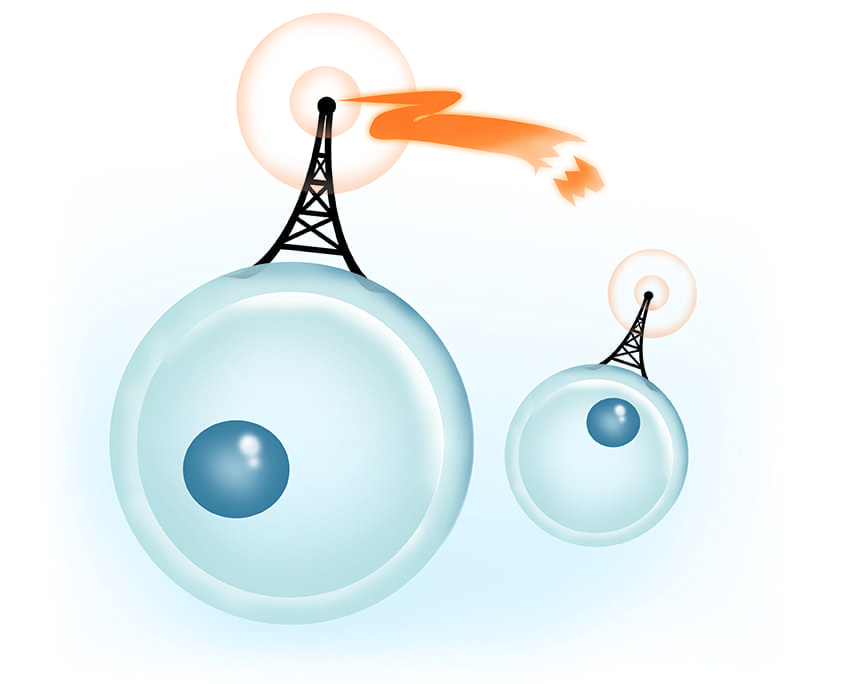
Why cell signaling matters: To fight an infection, different types of cells have to communicate and work together. This coordination relies on having well-functioning cell-surface receptors.
Stimulating a Healthy Immune Response
Receptors activate our immune cells. That’s why having well-functioning receptors improves the body’s ability to mount a healthy infection response and react more effectively to drugs and other treatments [11, 12]
How Omega-3s Have Performed in COVID-19 Trials
While the case for omega-3s is compelling from a theoretical standpoint, we know less about how these fatty acids act in clinical settings. While trials are underway, few studies have yet to be completed using omega-3 supplements as part of a COVID-19 treatment protocol.
At the time of publishing this article, here is what we know so far:
Higher Omega-3 Levels Linked with Reduced Mortality
Two studies to date have looked at how a person’s omega-3 levels correlate with COVID-19 severity. To assess the omega-3 levels, the researchers used the omega-3 index test to assess the amount of EPA and DHA in the patients’ red blood cells over the past four months.
• One pilot study surveyed 100 COVID-19 patients hospitalized at Cedars-Sinai Medical Center. After adjusting for age and sex, the researchers found that patients with lower omega-3 levels had a 75% increased risk of death compared to those with higher omega-3 levels [11].
• A second study from Chile found similar results when surveying 75 COVID-19 patients. Patients with the lowest omega-3 levels had 3.1-fold higher risk of dying compared to the patients with the highest levels. On the other hand, patients with the highest omega-3 levels were half as likely to need a ventilator [13].
The authors of both studies called for follow up research since the sample sizes were small. But their findings do lend credence to the hypotheses described above.
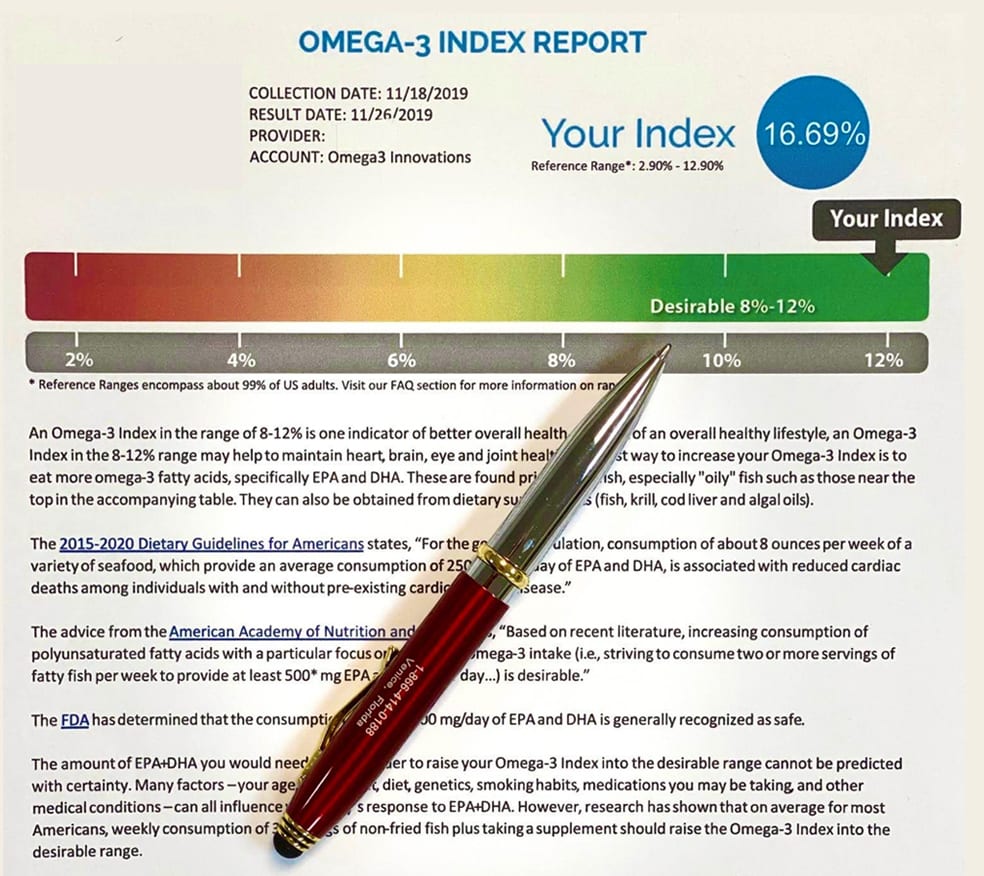
Got enough omegas? The omega-3 index is one of the best ways to measure EPA and DHA levels based on your intake over the last 4 months. Most Americans have omega-3 index scores in the undesirable 4% range.
Mixed Results for Omega-3 Supplements
The science is less clear for trials using omega-3s in acute clinical settings.
It is possible that the findings could be influenced by timing. After all, it typically takes 3 – 4 months before omega-3s become integrated in the body. Nonetheless, two completed studies have looked at how short-term omega-3 treatments impacted COVID-19 patients:
• In one double-blind clinical trial, the researchers gave 600 mg of EPA/DHA to 128 critically ill COVID-19 patients for 14 days. At the one-month mark, the omega-3 group had significantly better survival rates compared with the control group (21% vs. 3%). It should be noted that some scientists have questioned this study’s approach. Therefore, the results should be interpreted with caution [14].
• In another study of 2000 COVID-19 patients, the researchers gave 8000 mg of prescription EPA for 3 days and 4000 mg for the rest of the month. The omega-3 intervention trended towards reduced rates of hospitalization and death. But ultimately, it was not enough of a benefit to reach statistical significance compared to placebo [15].
Both trials offer hope. However, we need more long-term, larger-scale studies to draw conclusions at this time.
Omega-3s Matter, But We’re Still Learning
As essential fatty acids, omega-3s undisputedly impact our immune system. Their effects on lipid metabolism, inflammation, and cell signaling are not only relevant for COVID-19, but for lots of bacterial and viral infections. Still, as the research demonstrates, we have a lot to learn.
It is also important to remember that omega-3s represent only one aspect of wellness. As we’ll discuss further, other vital nutrients – like vitamin D and melatonin – also influence how our bodies respond to disease. (And so, of course, do factors like exercise, sleep, diet, etc.)
While omega-3s are but one piece of the puzzle, getting enough of these fats remains an important step on the journey to better health.
An Effective Omega-3 Dose, Made Simple
Experience the Omega3 Innovations difference for yourself with the most effective fish oil supplement on the market.
Buy Now
References:
1. Darwesh, A. M., Bassiouni, W., Sosnowski, D. K., & Seubert, J. M. (2021). Can N-3 Polyunsaturated Fatty Acids Be Considered a Potential Adjuvant Therapy for COVID-19-Associated Cardiovascular Complications? Pharmacology & Therapeutics, 219, 107703.
2. Weill, P., Plissonneau, C., Legrand, P., Rioux, V., & Thibault, R. (2020). May Omega-3 Fatty Acid Dietary Supplementation Help Reduce Severe Complications in Covid-19 Patients? Biochimie, 179, 275–280.
3. Arnardottir, H., Pawelzik, S. C., Öhlund Wistbacka, U., Artiach, G., Hofmann, R. et al. (2021). Stimulating the Resolution of Inflammation Through Omega-3 Polyunsaturated Fatty Acids in COVID-19: Rationale for the COVID-Omega-F Trial. Frontiers in Physiology, 11, 624657.
4. Rezaei, A., Neshat, S., & Heshmat-Ghahdarijani, K. (2021). Alterations of Lipid Profile in COVID-19: A Narrative Review. Current Problems in Cardiology, 100907. Advance Online Publication.
5. Hathaway, D., Pandav, K., Patel, M., Riva-Moscoso, A., Singh, B. M., Patel, A., Min, Z. C., Singh-Makkar, S., Sana, M. K., et al. (2020). Omega 3 Fatty Acids and COVID-19: A Comprehensive Review. Infection & Chemotherapy, 52(4), 478–495.
6. McReynolds, C. B., Cortes-Puch, I., Ravindran, R., Khan, I. H., Hammock, B. G., Shih, P. B., Hammock, B. D., & Yang, J. (2021). Plasma Linoleate Diols Are Potential Biomarkers for Severe COVID-19 Infections. Frontiers in Physiology, 12, 663869.
7. Nayeem M. A. (2018). Role of Oxylipins in Cardiovascular Diseases. Acta Pharmacologica Sinica, 39(7), 1142–1154.
8. Pal, A., Gowdy, K. M., Oestreich, K. J., Beck, M., & Shaikh, S. R. (2020). Obesity-Driven Deficiencies of Specialized Pro-resolving Mediators May Drive Adverse Outcomes During SARS-CoV-2 Infection. Frontiers in Immunology, 11, 1997.
9. Palmas, F., Clarke, J., Colas, R. A., Gomez, E. A., Keogh, A., Boylan, M., McEvoy, N., McElvaney, O. J. et al. (2021). Dysregulated Plasma Lipid Mediator Profiles in Critically Ill COVID-19 Patients. PloS One, 16(8), e0256226.
10. Theken, K. N., Tang, S. Y., Sengupta, S., & FitzGerald, G. A. (2021). The Roles of Lipids in SARS-CoV-2 Viral Replication and the Host Immune Response. Journal of Lipid Research, 62, 100129.
11. Asher, A., Tintle, N. L., Myers, M., Lockshon, L., Bacareza, H., & Harris, W. S. (2021). Blood Omega-3 Fatty Acids and Death from COVID-19: A Pilot Study. Prostaglandins, Leukotrienes, and Essential Fatty Acids, 166, 102250.
12. Hou, T. Y., McMurray, D. N., & Chapkin, R. S. (2016). Omega-3 Fatty Acids, Lipid Rafts, and T Cell Signaling. European Journal of Pharmacology, 785, 2–9.
13. Zapata B, R., Müller, J. M., Vásquez, J. E., Ravera, F., Lago, G., Cañón, E., Castañeda, D., Pradenas, M., & Ramírez-Santana, M. (2021). Omega-3 Index and Clinical Outcomes of Severe COVID-19: Preliminary Results of a Cross-Sectional Study. International Journal of Environmental Research and Public Health, 18(15), 7722.
14. Doaei, S., Gholami, S., Rastgoo, S., Gholamalizadeh, M., Bourbour, F., Bagheri, S. E. et al. (2021). The Effect of Omega-3 Fatty Acid Supplementation on Clinical and Biochemical Parameters of Critically Ill Patients with COVID-19: A Randomized Clinical Trial. Journal of Translational Medicine, 19(1), 128.
15. (2021, November 15). Prescription Omega-3 Pill Didn’t Affect Outcome for Non-Hospitalized Adults with COVID-19. American Heart Association Scientific Sessions 2021.
Popular posts


Related posts