COVID-19: Why Melatonin Research Matters
As the number of COVID-19 cases continues to rise close to home, it has set up hypochondriacal terror in my brain these past weeks. Despite exercising, eating lots of vegetables, meditating, wearing a mask whenever I’m in public, and incessantly washing my hands, I jump in panic whenever I hear someone coughing or sneezing.
To calm my nerves, I wanted to better understand how this invisible adversary behaves. And as a physician who’s spent years studying the effects of melatonin, I wondered if there might be any overlap between this natural hormone and COVID-19.
Why Is SARS-CoV-2 Such a Powerful Virus?
First of all, I am going to start with the bad news. COVID-19 is not something to take lightly, even if the curve is (thankfully) flattening in many states. Here are 5 reasons why:
1. COVID-19 Has “Sticking Power”
The job of a virus is to hijack cells and use the cell’s organelles to reproduce. They act sort of like pirates hopping aboard a ship and taking command. For this reason, how effectively the virus grabs onto the cells determines how well it spreads.
Say you’re walking through the grocery store and someone in front of you coughs. If you are in range, cough droplets may end up traveling into your nose or mouth. And if that droplet happens to contain the COVID-19 virus (also known as SARS-CoV-2), its crown-like spikes allow it to easily attach to your mucus membrane cells. These spikes are important to understand.
The SARS virus from 2003 shares about 79% of the same genetic structure as SARS-CoV-2 (1). But compared to the 2003 virus, the spike structure of SARS-CoV-2 allows it to stick much more strongly to receptors on the host-cell. Scientists think that this increased “sticking power” means that less virus needs to be present to start the infection (2).
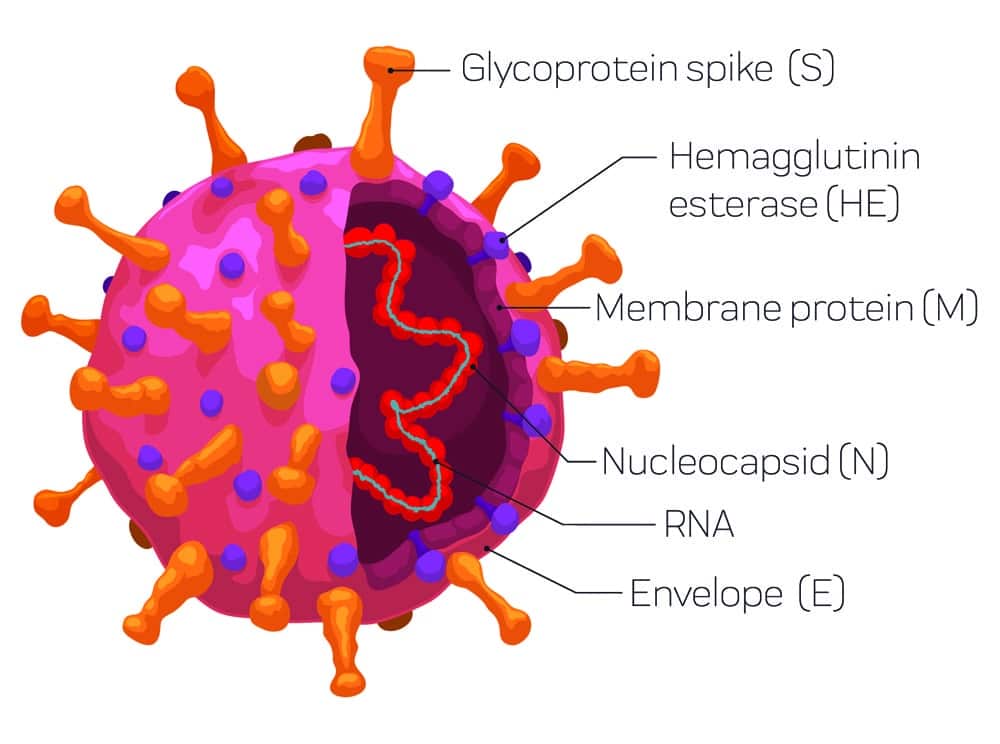
The structure of SARS-CoV-2, and the way it binds to the cells in our bodies, helps explain why it is such a formidable adversary.
2. COVID-19 Is Sneaky
The majority of those infected with COVID-19 feel some sort of symptoms, like a dry cough, malaise and fever. But people can have no or mild symptoms for up to two weeks, and therefore infect others unknowingly (3).
This is especially true of children, particularly those under the age of 9. The majority of them don’t seem to be weighed down with the more serious aspects of this disease compared to adults over the age of 60. While children can certainly be infected, their symptoms usually don’t manifest as double pneumonia like in adults (4).
3. COVID-19 Affects Upper & Lower Respiratory Systems & More
As mentioned above, SARS-CoV-2 is characterized by its crown-like spikes that it uses to attach to the cells in the mucus membrane. These spikes attach to a special receptor called Angiotensin Converting Enzyme 2, or ACE2 for short. In addition, the spikes also make use of a special enzyme called Furin.
Once the spikes of the virus attach to the ACE2 receptors on the cell membrane, the Furin enzyme chops the two halves of the spike in the middle. This action gives the virus greater stability and increases its ability to spread into the cell (5). Furthermore, because the ACE2 receptors are present in many of our cells, it provides SARS-CoV-2 the possibility of attacking multiple organs and different types of cells throughout our bodies (6).
This affinity for the ACE2 receptors and the Furin enzyme allows SARS-CoV-2 to attack not only the upper and lower respiratory system, but also the small intestines, liver, kidneys, and central nervous system (6). This is also likely why we are now hearing reports of COVID-19 patients with encephalitis, or inflammation of the brain (7).
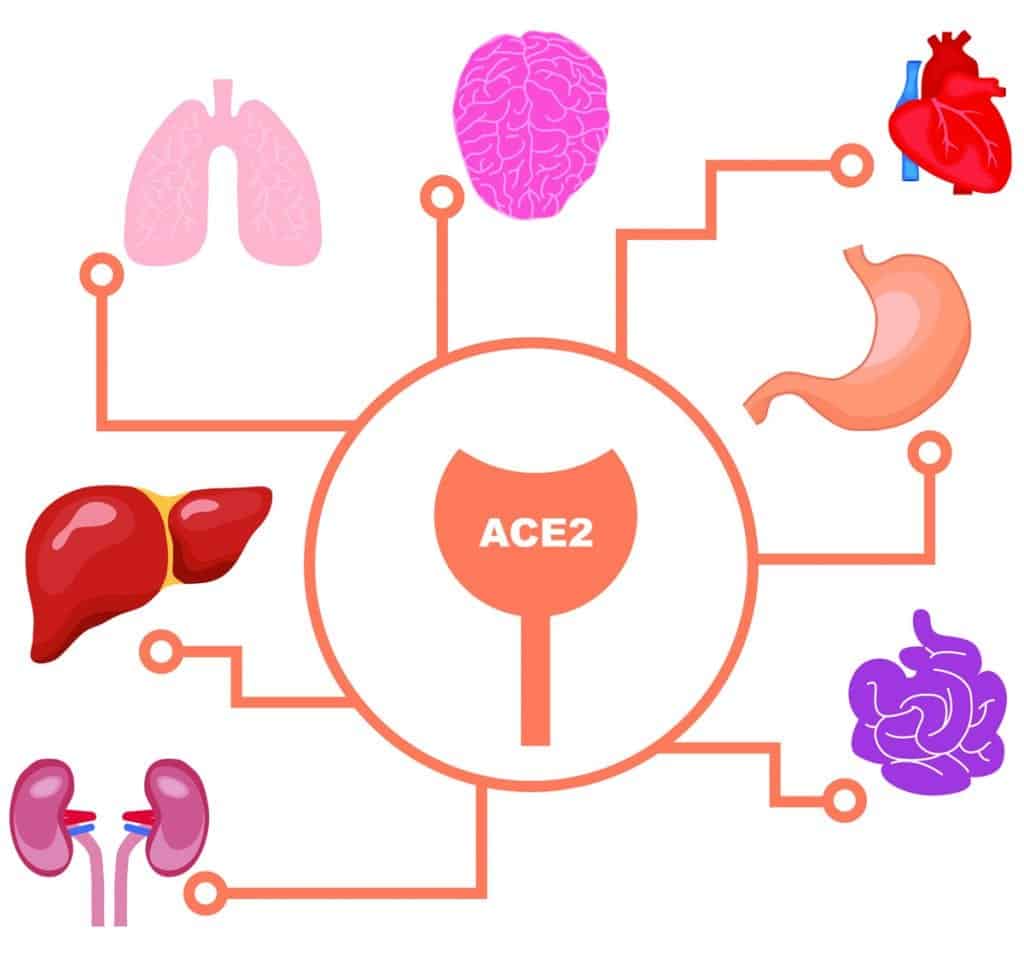
Many organs in the body – including the lungs, kidneys, small intestines, and brain – are rich in ACE2 receptors. Their widespread prevalence is one reason why scientists think COVID-19 can wreak havoc throughout the body.
4. COVID-19 May Have Lasting Health Effects
Besides the repercussions of the immediate infection (like scarring of the lungs), we will also likely see multiple after effects from COVID-19. For instance, a small 12-year follow-up study of those infected with SARS from 2003 found that 68% developed hyperlipidemia, 44% had cardiovascular system issues, and 60% had glucose metabolic disorders (8). Similarly, some researchers theorize that COVID-19 may accelerate aging and cause aging-associated disorders in the future (9).
Unfortunately, those who are especially at risk of COVID-19 complications are probably at greater risk of developing more severe residual effects from this infection, too.
5. SARS-CoV-2’s Structure Helps It Mutate
Compared to many other viruses, coronaviruses like SARS-CoV-2 are made up of a fairly long strand of genetic material (10). Why does this matter? Think about it like a password. It is easier to make mistakes when typing in a longer password. In the same way, it’s easier for the virus to make mistakes (or mutations) when replicating an extra long strand of RNA material.
The problem with mutations comes when scientists try to create a vaccine to match a particular strain of the virus. The faster a virus mutates, the more difficult it becomes to establish a workable vaccine (11).
Is There Any Good News About COVID-19?
One thing that has made me feel marginally better is reading some of the research surrounding melatonin — especially since this is a molecule that my husband, Dr. Bo Martinsen, and I have spent several years studying, in conjunction with omega-3s.
I have seen some news sites and commentators buzz about the potential effects of melatonin for COVID-19, but typically with very little context and limited information. So, let me take a moment to highlight the research currently available on the topic:
The Potential Effects of Melatonin on COVID-19
Among numerous other substances, melatonin is currently being investigated for its potential effects on COVID-19 (both by itself and in conjunction with other treatments).
As we’ve tackled in previous articles, melatonin has a multitude of health-promoting properties beyond treating sleep disorders. For instance, past research has documented the positive effects of melatonin for alleviating acute respiratory stress caused by viruses, bacteria, and radiation (12).
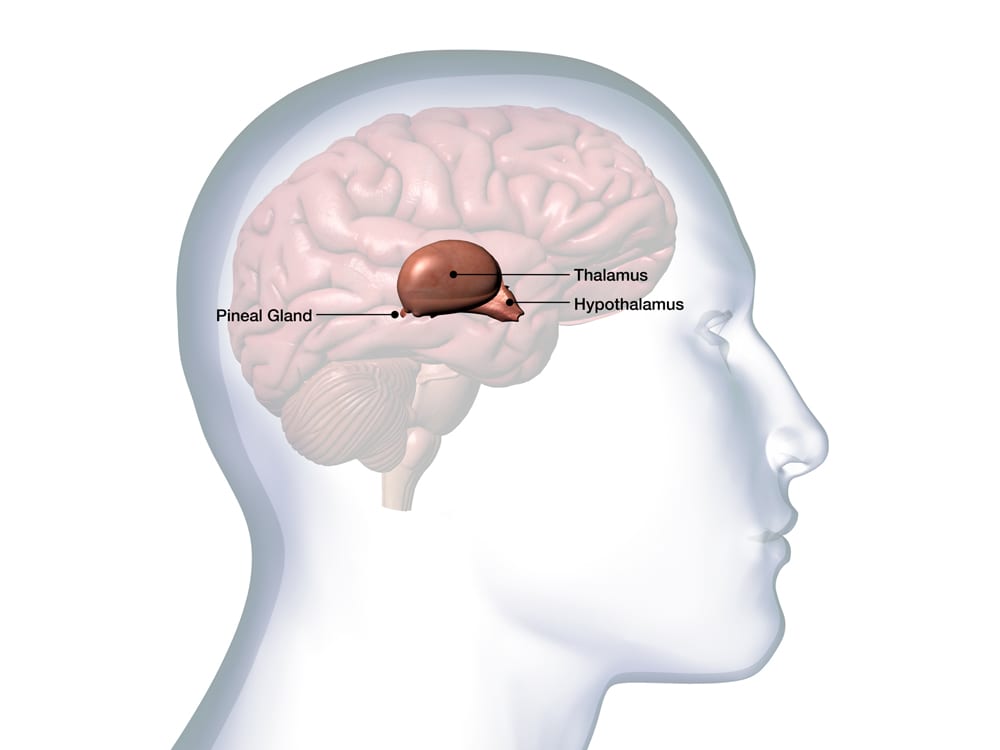
In addition to being secreted by the pineal gland at night, melatonin is also found in every cell in the body. It carries out a wide range of antioxidant and anti-inflammatory functions – as well as regulates sleep.
Professor Russel Reiter, one of the grandfathers of melatonin research, recently co-authored a paper with scientists from China. Together, they presented the theoretical reasons for why melatonin may be an effective adjuvant in reducing Acute Lung Injury (ALI) and Acute Respiratory Distress Syndrome (ARDS) induced by SARS-CoV-2. That said, their hypotheses have not yet been tested in COVID-19 clinical studies.
You can read the article in full here. Below are some key points from the article:
Melatonin Reduces Inflammation
Melatonin does not kill viruses, but it may help stem viral infections’ more harmful effects by influencing the cytokines (12). Normally, cytokines are like soldiers fighting off the bad guys; they help create an inflammatory response that kills harmful microbes in the body.
During certain types of viral infections, however, cytokines may have both antiviral and proviral effects. This means that they can both inhibit viral replication and reduce the infection OR facilitate the infection by negatively impacting the immune response (13, 14, 15).
In some cases, the overproduction of some proinflammatory cytokines can do more harm than good, potentially even leading to a “cytokine storm.”
Melatonin reduces levels of pro-inflammatory cytokines and chemokines, including interleukin-6 (IL-6) (12). Since cytokine storms seem to be one of the killers in a COVID-19 infection, this could be potentially beneficial (16).
Melatonin Has Antioxidant Properties
Melatonin is one of nature’s most potent antioxidants, and that antioxidant effect could potentially spell good news for patients: When you have a viral infection, the infection causes a rapid increase in oxidized products within your body.
Having an increase in oxidative stress in the body is generally harmful, since it can contribute to cell and tissue damage. For COVID-19 patients, oxidation products may have additional significance: In SARS-oriented Acute Lung Injury models (ALI), researchers found that the overproduction of oxidation products contributed to increased inflammation that led to ALI (12).
For these reasons, it’s thought that reducing the amount of oxidation products via antioxidants like melatonin could be helpful in mitigating damage.
Melatonin May Have Other Benefits
Besides its effects on inflammation and oxidation, the researchers also theorize that melatonin could make patients more comfortable during treatment, thanks to its effects on pain, anxiety and sleep (12).
How Much Do We Know About Melatonin and COVID-19?
As mentioned, in the above referenced article, researchers are trying to present the case for why they think melatonin could work for COVID-19. But because SARS-CoV-2 is only a few months old, there’s simply not enough data about how it might work in practice yet.
It’s important to remember that – when it comes to any kind of illness – it’s not enough to have a hypothetical rationale for why certain treatments might work: You must put it to the test with controlled, randomized trials.
At the time of writing this article, there are still no COVID-19 drugs or other therapeutics (either for prevention or treatment) approved by the US Food and Drug Administration.
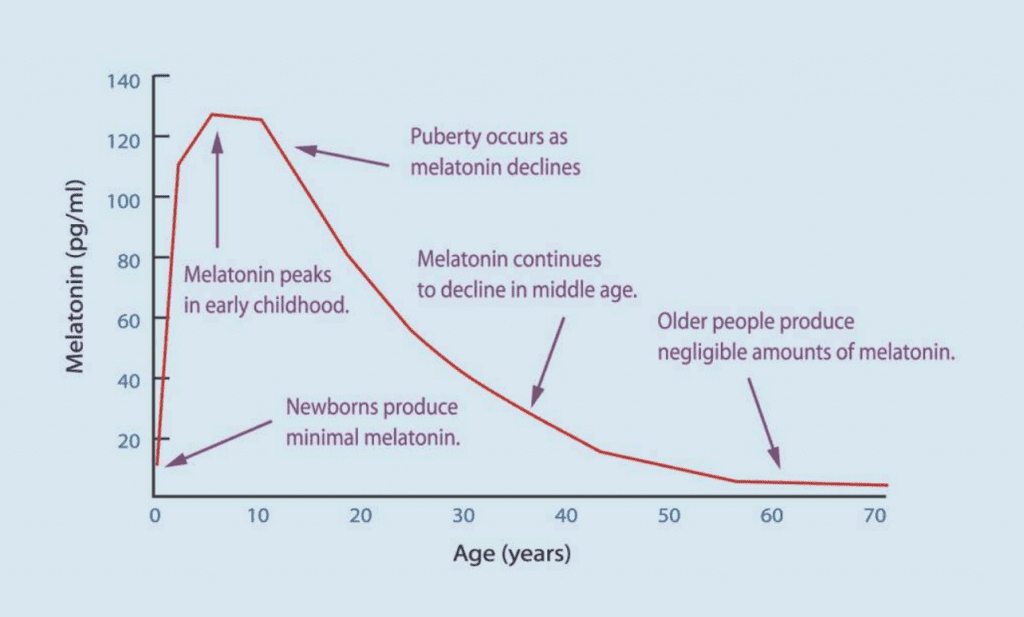
The body’s natural melatonin production declines with age. Source: Grivas, T. B., & Savvidou, O. D. (2007). Melatonin the “Light of Night” in Human Biology and Adolescent Idiopathic Scoliosis. Scoliosis, 2, 6.
Why Melatonin Is a Good Choice for Trials
Melatonin, fortunately, has a strong safety record with few serious adverse effects. Additionally, most viruses seem to actively inhibit melatonin production in the body, suggesting this natural hormone has an important role in regulating viral infections (17). Both of these factors make melatonin a compelling option to explore.
Already, some practitioners are working to determine what melatonin treatment might look like in real life. There are reports of doctors in the Philippines studying the effects of high-dose melatonin on COVID-19 patients, as well as a doctor in Texas who is similarly using high doses for patients in his practice.
We hope to have more information about melatonin’s effects on COVID-19 in the coming months.
Good Health Comes from a Broader Approach
There’s one last point that also gives me some comfort in all of this: There are many different nutrients and drugs being considered for COVID-19 treatment. Even more encouraging, many of them will likely be successful, since there are multiple ways of targeting this virus. For instance, vitamin D is also receiving a lot of attention, and we’ll cover some of that research in depth in our next blog.
Due to the complexity of the human body, however, there’s almost never a single substance that can “do it all.” That’s why a synergistic approach to health — including improving diet and increasing exercise — often works the best.
I hope that this article brings you the same comfort and knowledge that I got from writing it. Be safe and well, dear friends.
An Effective Omega-3 Dose, Made Simple
Experience the Omega3 Innovations difference for yourself with the most effective fish oil supplement on the market.
Buy Now
References:
1. Lu, R., Zhao, X., Li, J., Niu, P., Yang, Bo., Wu, H. et al. (2020). Genomic Characterisation and Epidemiology of 2019 Novel Coronavirus: Implications for Virus Origins and Receptor Binding. The Lancet, 395(10224): P565-574.
2. Sandoiu, A. (2020, March 17). Why Does SARS-CoV-2 Spread So Easily? Medical News Today.
3. (2020, April 4). No Signs of Coronavirus? Here’s Why You Could Still Be Carrying (and Spreading) It. Health Essentials. Cleveland Clinic.
4. Ludvigsson, J. F. (2020). Systematic Review of COVID‐19 in Children Shows Milder Cases and a Better Prognosis Than Adults. Acta Paediatrica, 2020(00): 1– 8.
5. Thomas G. (2002). Furin at the Cutting Edge: From Protein Traffic to Embryogenesis and Disease. Nature Reviews: Molecular Cell Biology, 3(10), 753–766.
6. Wadman, M., Couzin-Frankel, J., Kaiser, J. & Matacic, C. (2020, April 17). How Does Coronavirus Kill? Clinicians Trace a Ferocious Rampage Through the Body, from Brain to Toes. Science.
7. Talan, J. (2020, April 1). First Case Report of Acute Necrotizing Encephalopathy Associated with COVID-19. Neurology Today.
8. Wu, Q., Zhou, L., Sun, X., Yan, Z., et al. (2017). Altered Lipid Metabolism in Recovered SARS Patients Twelve Years after Infection. Scientific Reports, 7(1), 9110.
9. Lippi, A., Domingues, R., Setz, C., Outeiro, T.F. & Krisko, A. (2020). SARS‐CoV‐2: At the Crossroad Between Aging and Neurodegeneration. Movement Disorders.
10. Makin, S. (2020, February 5). How Coronaviruses Cause Infection—from Colds to Deadly Pneumonia. Scientific American.
11. Lash, N. & Schlossberg, T. (2020, April 16). The Coronavirus Is Mutating. What Does That Mean for a Vaccine? The New York Times.
12. Zhang, R., Wang, X., Ni, L., Di, X., Ma, B., Niu, S., Liu, C., Reiter, R. J. (2020). COVID-19: Melatonin as a Potential Adjuvant Treatment. Life Sciences, 250.
13. Loh, D. (2020, March 14). COVID-19, Pneumonia & Inflammasomes – The Melatonin Connection. Evolutamente.
14. Velazquez-Salinas, L., Verdugo-Rodriguez, A., Rodriguez, L. L., & Borca, M. V. (2019). The Role of Interleukin 6 During Viral Infections. Frontiers in Microbiology, 10, 1057.
15. McGonagle, D., Sharif, K., O’Regan, A. & Bridgewood, C. (2020). The Role of Cytokines Including Interleukin-6 in COVID-19 Induced Pneumonia and Macrophage Activation Syndrome-Like Disease. Autoimmunity Reviews, 102537.
16. Brumfield, G. (2020, April 7). Why Some COVID-19 Patients Crash: The Body’s Immune System Might Be To Blame. NPR: Morning Edition.
17. Anderson, G. & Reiter, RJ. (2020). Melatonin: Roles in Influenza, Covid‐19, and Other Viral Infections. Reviews in Medical Virology, e2109.
Popular posts


Related posts